

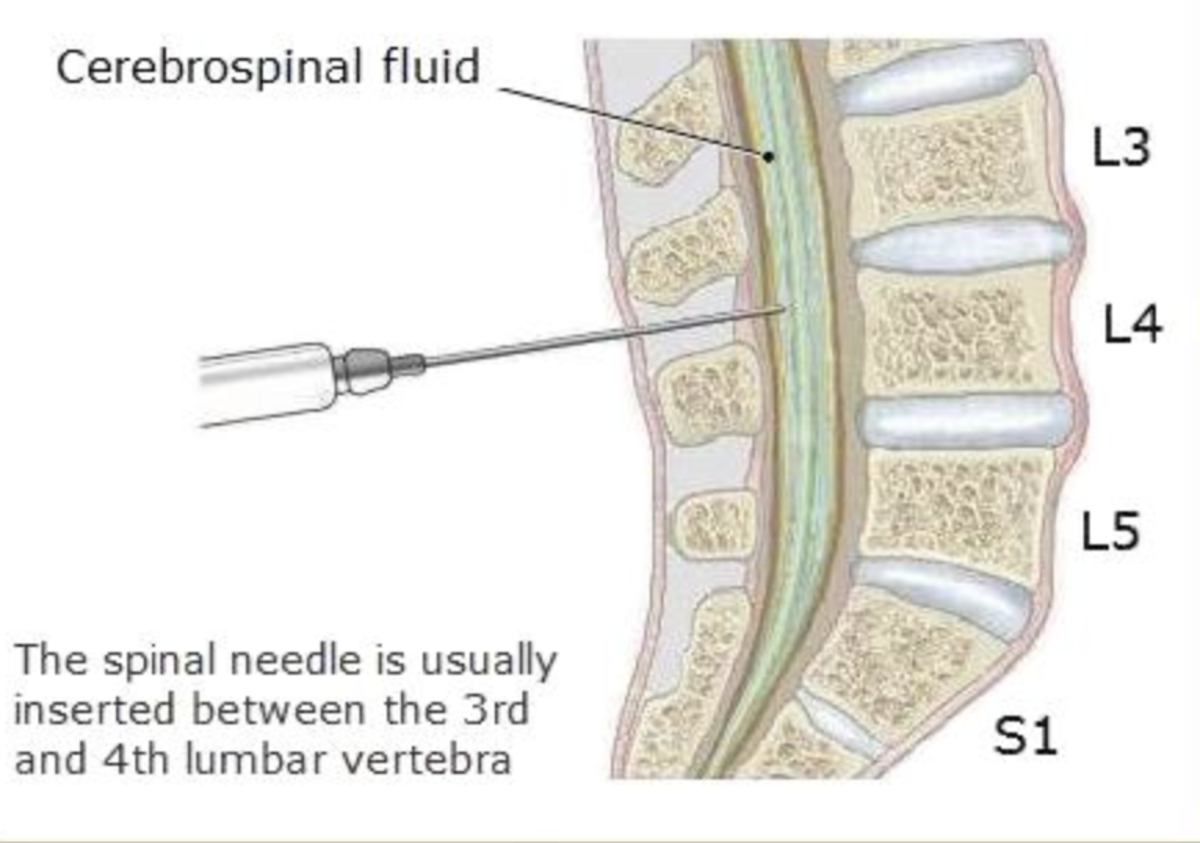
Less frequently, a lumbar puncture can be done as a means of treatment if a person has too much CSF, and the pressure of the fluid around the brain and spine is too high. They will also check the pressure of the CSF. Doctors may look for changes in the fluid that could indicate infection or bleeding, or unusual or uncommon cells that could be a sign of a neurological disorder. Often, a lumbar puncture is done because doctors need to do some tests on the CSF to help them make a diagnosis. It is sometimes referred to as a spinal tap.
#Side effects after lumbar puncture Patch#
All cases reported received a lumbar epidural blood patch that was always curative.A lumbar puncture involves extracting some of the fluid that surrounds your brain and spine (known as cerebrospinal fluid or CSF).
Two cases of postdural puncture thoracic pain were reported by Dunbar, 11one after an inadvertent lumbar puncture, another after a cervical puncture, both, as in the current scenario, for therapeutic steroid injection. 10reported a case of arm pain with dysesthesia after an unintended dural puncture, and explained it as irritation of the C5 and C6 nerve roots caused by central traction. McGrady and Freshwater 9reported a case of posterior neck pain (C2–4) without headache after spinal anesthesia. Neck stiffness is frequently reported (43%), always together with headache. 4classified the PDPH based on the intensity and characteristics of the cephalalgia, and cited the interscapular pain as “related musculoskeletal symptom,” however, no instances of upper back pain are cited among the 75 cases of PDPH reported by the authors. Discussionįew cases of atypical postdural puncture symptoms have been reported in the literature. In a follow-up examination 4 months after the steroid injection, the patient had significant improvement of the lumbar radicular pain, and the upper back pain had disappeared. The neck pain recurred throughout the next 2 months but paracetamol 500 mg taken orally was enough to control it. The patient was totally asymptomatic 24 h later. After 15 ml of blood was injected the dorsal pain disappeared, and after 20 ml the neck pain had almost completely gone. Under sterile conditions an epidural blood patch was performed at L2–元 with 20 ml blood injected through an 18-gauge Tuohy needle. The dorsal pain recurred, and 72 h after the procedure an epidural blood patch was proposed to the patient (additional caffeine was not accepted). After orally taking 300 mg caffeine the patient developed great anxiety and insomnia, with a slight improvement in the intensity of the pain. A PDPH syndrome was suspected because the symptoms increased when the patient was in the upright position. The pain was described as severe, continuous, interscapular pressure without radiation. Forty-eight hours after the procedure light neck pain with stiffness developed, along with severe incapacitating upper back pain. Twenty-four hours later the patient complained of moderate upper back pain that was attributed to anxiety and muscle spasm.

#Side effects after lumbar puncture plus#
Paracetamol 500 mg plus codeine 30 mg taken orally twice a day, and copious liquid intake was recommended. The asymptomatic patient was discharged home with written instructions to contact the clinic in case of headache or other symptoms. Intravenous paracetamol 2,000 mg and 1,500 ml lactated Ringer's solution were given. The patient was asked to remain supine for 2 h. The steroid injection was eventually performed one space above. In the second block an accidental dural puncture at 元–4 occurred. During the first epidural injection the patient had a vasovagal syncope that was treated with 1 mg intravenous atropine. The drugs used were paramethasone 40 mg diluted in 4 ml bupivacaine, 0.25%. The epidural procedure was performed with an 18-gauge Tuohy needle, with loss of resistance to air technique, in the 元–L4 interspace. They were performed in an ambulatory setting. Two epidural steroid injections were proposed and accepted as initial treatment. Magnetic resonance imaging showed vertebral disk herniation at the L2–元, 元–L4, and L4–L5 levels and sacralization of L5. His physical examination revealed an obese and anxious patient with acute lumbalgia (acute lumbar pain). His medical history revealed previous opioid addiction, chronic hepatitis B and C, knee arthritis, dislipemia, and heavy smoking. A 39-yr-old, 92 kg, 170 cm man presented to our pain clinic with severe lumbar pain accompanied by radicular symptoms.


 0 kommentar(er)
0 kommentar(er)
